Introduction
Millions of individuals worldwide suffer from osteoarthritis, the most prevalent kind of arthritis. It happens as the connective tissue that cushioning both ends of each bone ages and becomes less effective. Although osteoarthritis can affect any joint, it most commonly affects the spine, hands, knees, and hips. Osteoarthritis symptoms may usually be controlled, despite the irreversible nature of joint deterioration. Remaining physically active, keeping a healthy weight, and undergoing specific therapies may assist to reduce discomfort and enhance joint function while also slowing the disease’s progression.
Causes
The slow deterioration of the cartilage that cushioning both ends of the bones in your joints can lead to osteoarthritis. Joint mobility is nearly frictionless because of cartilage, a strong, smooth material. Bone will eventually rub against bone if the cartilage breaks out completely. For osteoarthritis, the phrase “wear and tear syndrome” is commonly used. However, osteoarthritis damages the entire joint in addition to the cartilage deterioration. It results in alterations to the skeletal structure as well as degradation of the connective cells that stabilize the joint and bind muscle to bone.
Types of Osteoarthritis
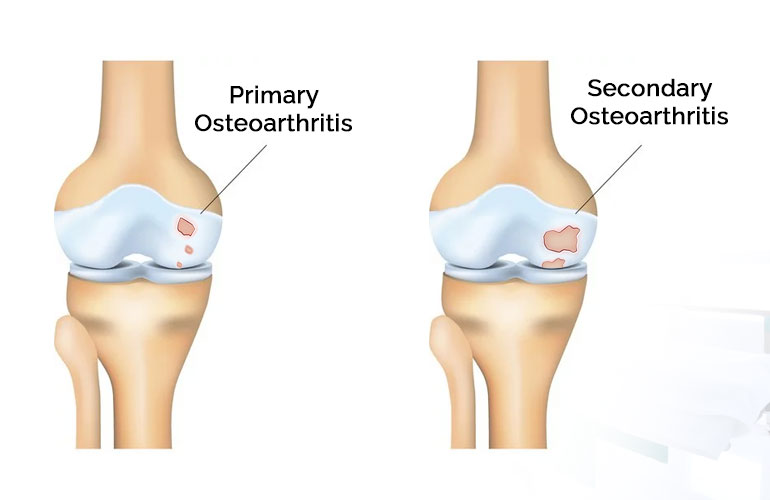
Your osteoarthritis may be classified as primary or secondary by your physician.
Primary Osteoarthritis:
Over time, primary arthritis develops. According to experts, it’s brought on by the deterioration of your joints from daily use.
Secondary Osteoarthritis:
An damage to one of your joints leads to secondary arthritis.
Tricompartmental Osteoarthritis:
Your knee is affected by this type of osteoarthritis. There are three compartments in that joint: patellofemoral, lateral, and medial. The side of your knee that is nearest to your other knee is called the medial compartment. The outside of your knee is called the lateral compartment. The side of your knee is called the patellofemoral. Any of these categories may be impacted by arthritis. It’s called tricompartmental osteoarthritis when any three are afflicted.
Erosive Osteoarthritis:
This form, also known as EOA, typically affects the hand joint. Osteoarthritis (EOA) is an aggressive kind of the disease that affects the “interphalangeal” joints in your fingers, which are the hinges that allow you to produce fists and other movements. Your afflicted joints will be heated, red, and swollen if you have EOA. It is referred to as inflammatory arthritis for this reason. You’ll be in discomfort and unable to move very much. In rare cases, it may also impact the shoulders, hips, and feet.
Additional Forms of Osteoarthritis:
Hip Osteoarthritis
You experience hip joint discomfort and stiffness when osteoarthritis damages this joint. It may also be felt in your inner thighs, butt, or groin. On occasion, the soreness may spread to your knee. Your hip range of motion will decrease as the problem worsens.
Spondylosis
Your spine is impacted by this kind of osteoarthritis. Your spine as a whole may be affected. Your back’s disks may start to deteriorate, and bone spurs, also known as osteophytes, may develop on your spine. Bone spurs or weakened disks might compress your back’s nerves. Spinal stenosis, a narrowing of the opening where the vertebral column and other vital nerves pass, can develop as spondylosis gets worse. Your arms and shoulders may hurt or become numb, depending on which area of the spine is impacted. Your legs can hurt or become numb if the harm is deeper down. Learn More About Spondylosis.
Shoulder Osteoarthritis
The glenohumeral joint, which is a ball and socket joint in the shoulder, is the primary joint affected by arthritis. The acromioclavicular a joint, a second location in your shoulder, may also be impacted. It is referred to as AC joint arthritis when that occurs. Shoulder pain, sometimes even when the shoulder is not being used, is the primary symptom of this illness. You may also have a grinding or stiff shoulder, as well as joint noises like cracking or popping. We name that crepitus.

Sign And Symptoms
The degree of your osteoarthritis and the area of your body that is affected will determine the symptoms you experience. The following are some of the most typical signs of arthritis:
- Joint discomfort
- Inflammation of the joints
- Reduction in adaptability
- Shortened range of motion
- Stiffness in the affected joint
- Additional masses of bone called bone spurs are usually painless
- Discomfort or tenderness when applying pressure with your fingertips to the afflicted areas
- Crepitus, which is the gritty, snapping, clicking, or popping noises produced by moving your joints
The pain related to osteoarthritis may worsen as the condition progresses. Inflammation in the joint itself and its environs may also develop with time.
Diagnosis
- A degenerative disease that typically progresses gradually is arthritis. Early on, it could be challenging to make an accurate diagnosis.
- After performing a physical examination, a medical expert will inquire about the symptoms and medical background.
- After that, they could request imaging tests like an MRI or X-ray to get a closer look at your joints.
- Sometimes a doctor will conduct an examination of synovial fluid (the fluid around the joints) or an ESR blood test to rule out other possible causes of inflammation or joint discomfort.
Treatment
Arthritis has no known cure, however treatment aims to Reliable Source:
- Alleviate the symptoms
- Lessen inflammation
- Improve your standard of living
- Improve the function, mobility, and flexibility of joints
The most suitable therapy plan for you might be created with assistance from a medical practitioner. Depending on a number of variables, including the location and intensity of your symptoms, this could differ for each person.
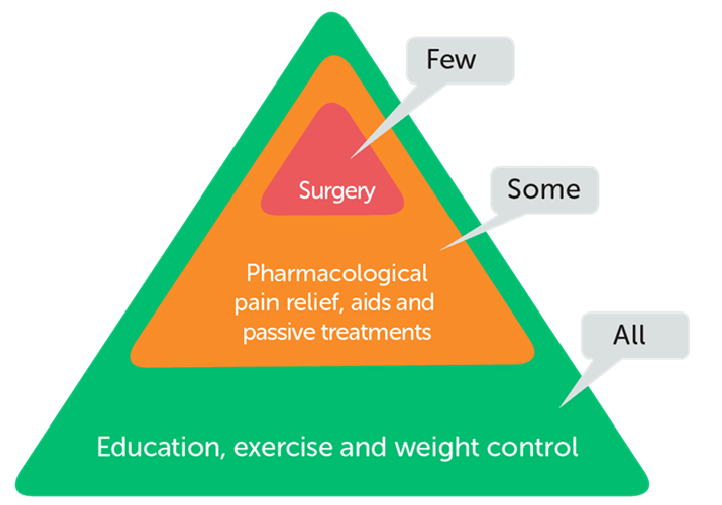
A combination of treatments will usually be part of your osteoarthritis treatment plan. These could consist of:
- Physical rehabilitation
- Aids and equipment, including knee braces
- Procedures like osteotomies and complete knee replacements
- Lifestyle adjustments, including better sleep, exercise, and weight control
- Changing one’s diet to include things like anti-inflammatory foods
- Natural therapies, including heat and cold treatments, yoga, and vitamins
- OTC pharmaceuticals, like nonsteroidal anti-inflammatory medicines (NSAIDs),
- Pharmaceuticals on prescription, like corticosteroids
3 comments