Introduction
Diabetic neuropathy is a type of nerve damage that can occur with long term uncontrolled diabetes. Hyperglycemia can injure nerves throughout the body. Diabetic neuropathy most often damages nerves in legs and feet affecting the longer sensory neurons first. Diabetic neuropathy is a common and serious complication of diabetes. But tight blood sugar control and a healthy lifestyle can prevent diabetic neuropathy or slow its progression.
Sign & Symptoms
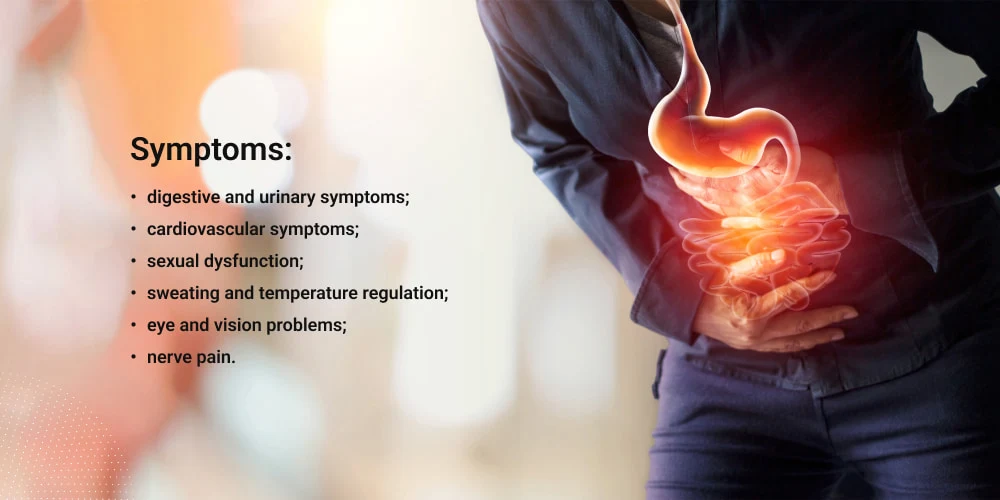
Depending on the affected nerves, symptoms of diabetic neuropathy can range from pain and numbness in the legs and feet to problems with digestive system, urinary tract, blood vessels and heart. Some people have mild symptoms. However, may find diabetic neuropathy to be extremely painful and incapacitating.
Types of Neuropathy
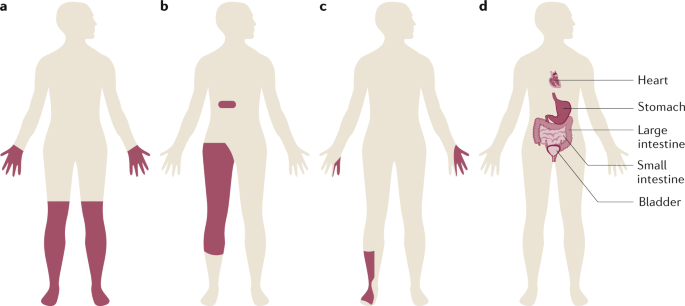
There are four main types of diabetic neuropathy. A person can have one or more than one type of neuropathy. Symptoms will depend on the type. Usually, symptoms develop gradually. Diabetic neuropathy is clinically silent until considerable nerve damage has occurred.
Peripheral Sensorimotor symmetric Neuropathy
Peripheral neuropathy is the most common type of diabetic neuropathy. Usually, these symptoms are worse at night. Peripheral neuropathy symptoms can include:
- Numbness or decreased feeling of pain or temperature changes
- Tingling or burning sensation
- Sharp pains or cramps
- Muscle weakness
- Loss of reflexes particularly in the ankle
- Lack of balance and coordination
- Serious foot issues like ulcers and infections
- Pain in the bones and joints.
- More responsiveness to touch (some people find that the pressure of a bedsheet can cause pain)
Autonomic Neuropathy
Injury to the nerves that regulate the body’s automatic processes results in autonomic neuropathy. Blood pressure, digestion, temperature regulation, bladder function, and even sexual activity may all be impacted. The signals that travel from the brain to various organs and autonomic nervous system regions are impacted by the injury to the nerves. The heart, blood vessels, and sweat glands are some of these regions. The most frequent reason for autonomic neuropathy is diabetes. Infections with germs or viruses, certain drugs, and other medical disorders might potentially be the reason. Treatment and symptoms differ according on the injured nerve. Damage to autonomic nervous system may cause:
- Difficulty swallowing
- Resting tachycardia
- Erectile dysfunction
- Vaginal dryness
- Increased or decreased sweating
- Problems controlling body temperature
- Constipation, uncontrolled diarrhea or both
- A lack of awareness that blood sugar levels are low (hypoglycemia unawareness)
- Bladder problems, including urinary tract infections or urinary retention or incontinence
- Slow stomach emptying (gastro paresis), causing nausea, vomiting, bloating and anorexia
- Sharp drops in blood pressure after sitting or standing that may cause fainting or feel lightheadedness
Radiculoplexus Neuropathy
Neuropathy affecting the radiculoplexus affects the thighs, hips, legs, and buttocks. It is more prevalent in older folks and those with type 2 diabetes. This form is also known as proximal neuropathy, femoral neuropathy, or diabetic amyotrophy. Usually affecting a single part of the body, symptoms can occasionally transfer to the other. Symptoms of radiculoplexus neuropathy include:
- Eventual weak and shrinking thigh muscles
- Difficulty rising from a sitting position
- Abdominal swelling, if the abdomen is affected
- Severe pain in a hip and thigh or buttock that occurs in a day or more
- Loss of weight Though symptoms can worsen before they get better, most people gradually get well
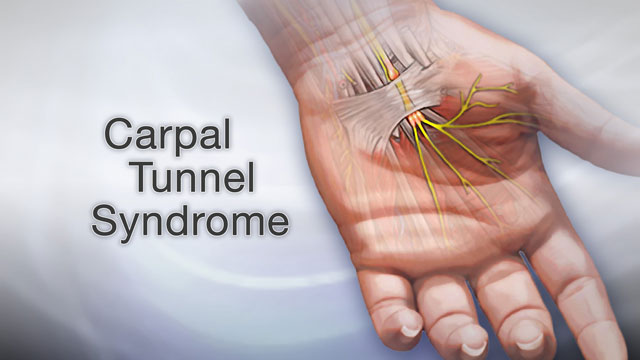
Mononeuropathy
Damage to a particular neuron in the face, torso or leg is known as mononeuropathy. It most frequently affects older persons. Mononeuropathy can cause excruciating pain and frequently hits suddenly. However, it usually doesn’t cause any long-term problems for example paralysis on one side of face (Bell’s palsy), double vision, pain in Shin or foot, Lower back or pelvis, Front of thigh etc. Sometimes mononeuropathy occurs when something is pressing on a nerve (nerve compression).
Diagnosis
The causes of peripheral neuropathy might be numerous. In addition to a physical examination, which could involve blood testing, diagnosis typically calls for:
An Exhaustive Medical Background
Your healthcare provider will review your medical history.. Your symptoms, way of life, exposure to chemicals, drinking patterns, and any family history of neurological or nervous system disorders will all be covered in the history.
Neurological Assessment
Your care provider may examine your muscular strength and tone, balance and coordination, capacity to perceive specific sensations, and tendon reflexes for diabetic neuropathy.
Tests
A medical practitioner may prescribe any of the following tests:
Blood Examinations
These can identify vitamin deficiency, diabetes, inflammatory markers, or metabolic problems that may lead to peripheral neuropathy.
Imaging Examinations
Herniated disks, nerve compression (also known as compressed nerves), growths, and other issues affecting bloodstream vessels and bones can all be seen with CT or MRI scans.
Testing of Nerve Function
To detect nerve injury, electromyography (EMG) analyzes and logs the electrical impulses in your muscles. To assess the electrical activity of a muscle contraction, a tiny needle, or electrode, is placed into the muscle. Usually, a nerve conduction examination is carried out in conjunction with an EMG. The skin is covered with flat electrodes, and the nerves are stimulated by a small electric current. How the nerves react to the current of electricity will be noted by a medical expert.
Additional Nerve Function Tests
A screen for autonomic reflexes may be among them. This examination documents autonomic nerve fiber function. Further tests might involve a sensory test that records your feelings of touch, vibration, chilling, and heat, as well as a sweat test that gauges your body’s capacity to sweat.
Biopsy of the Nerve
In an attempt to identify the source of the neuropathy, a tiny section of a nerve, typically a sensory nerve, is removed in this procedure.
Biopsy of the Skin
To count the amount of nerve endings, a tiny piece of skin is excised

3 comments